- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 5: e1. DOI 10.35630/2199-885X/2022/12/5.7
The study goal was to investigate hemodynamic parameters in medical students with different types of hemodynamics and their relationship with the body mass index.
Materials and methods. A cross-sectional study of 2- and 3-year students of the North-Ossetian State Medical Academy (NOSMA) (133 female and 37 male subjects) was performed. Blood pressure, pulse rate, and anthropometric variables were measured. Hemodynamic parameters and body mass index were calculated. Statistical processing included frequency and correlation analyses and analysis of variance.
Results. Overall, 60.6%, 36.5%, and 2.9% of the subjects had a eukinetic, hypokinetic, and hyperkinetic type of hemodynamics, respectively. Stroke volume (74.1 (68.6; 79.4)), cardiac output (7.8 (7.6; 7.8)), heart rate (100.4 (96.5; 109.9)), pulse pressure (50.0 (45.0; 60.0)), and rate pressure product (103.5 (90.3; 113.1)) were the highest in the hyperkinetic type group, and the lowest values of stroke volume (55.2 (54.2; 60.6)), cardiac output (4.3 (4.1; 5.0)), and pulse pressure (39.0 (30.0; 40.0)) were reported in the hypokinetic type group. Correlations between the evaluated parameters and body mass index (r=0.17–0.46) have been established. In the hypokinetic and eukinetic type groups, CO, SBP, DBP, PP, RPP, and AP were higher in subjects with BMI ≥ 25 compared with those with BMI < 25.
Conclusions. The eukinetic type of hemodynamics is the most common among medical students, and is predominantly inherent in females, while the hypokinetic type is more common among males. HR, SV, CI, CO, PP, RPP, KI increased and TPVR, RPVR, SBP, DBP, MBP decreased from the hypokinetic to hyperkinetic types. The observed within-group trends in the evaluated hemodynamic parameters were consistent with the types of hemodynamics both in female and male subjects. Regardless of the type of hemodynamics, the hemodynamic parameters and adaptation potential of the cardiovascular system decrease in subjects with BMI ≥ 25. Higher BMI was associated with a significantly greater cardiovascular load and AP of the cardiovascular system.
Keywords: types of hemodynamics, cardiovascular system, students, body mass index.
Establishing the type of circulation is an important step of the cardiovascular examination in patients with cardiovascular disease and healthy individuals. Adequate blood circulation ensures the normal functioning of internal organs. Early adaptation of hemodynamics and cardiovascular structures to external factors is the key to the optimal functioning of the body. Dysregulation of the cardiovascular system results in arterial dystonia and an imbalance between peripheral vascular resistance and cardiac output. Severe local and systemic disorders are known sequelae of systemic hemodynamic disturbances [1]. Analysis of hemodynamic parameters enables a correct assessment of the hemodynamic features of disease. Hemodynamic parameters may vary significantly in healthy individuals under conditions close to the basal metabolic rate [2, 3]. Although genetic variability of hemodynamic parameters has been demonstrated [4, 5], there is an opinion supporting relative stability of the regulation and patterns of cardiovascular (CV) response [6]. The metabolic status significantly affects the functioning of the cardiovascular system (CVS). Study load in medical universities has significantly increased and students have no time to keep a healthy diet. The predominance of carbohydrate-rich foods and active consumption of fast food predispose to metabolic disorders including weight gain which is a predictor of cardiovascular disease in adulthood. For this reason, a study of the relationship between hemodynamic parameters and body mass index (BMI) in students with different hemodynamic types would have undisputed theoretical and practical relevance.
The study goal was to investigate the hemodynamic parameters in medical students with different types of hemodynamics and their relationship with the body mass index and adaptation potential.
One hundred seventy NOSMA students (2- and 3-year) who were informed about the study goals and methods and signed informed consent comprised a simple random sample of a clinical, observational, cross-sectional study. The study was approved by the Ethics Committee of the Institute of Biomedical Research of the Vladikavkaz Scientific Center of the Russian Academy of Sciences (protocol No. 7 of February 20, 2019). The study is registered at ClinicalTrials.gov (NCT04851080). Healthy individuals were eligible and subjects with cardiovascular disease were excluded from the study. Thirty-seven males (mean age 20.7 ± 0.24 years) and 133 females (mean age 20.1 ± 0.07 years) preparing for exams were evaluated during spring and summer. Anthropometric variables (body weight and length), morning resting pulse rate (HR) and blood pressure (BP) were measured. HR was measured using a CMS 50DL pulse oximeter. BP was measured twice with a 2-minute interval by the auscultatory method. When BP measurements differed by > 5 mmHg, BP was remeasured after 2 minutes, and the arithmetic mean of the last two measurements was calculated. Based on the data collected, the following hemodynamic parameters were calculated using widely accepted calculation methods [7]: pulse pressure (PP, mmHg), mean blood pressure (MBP, mmHg), stroke volume using the formula (SV, mL), cardiac output (CO, L/min), rate pressure product (RPP, Robinson index), cardiac index (CI, L/min/m2), total peripheral vascular resistance (TPVR, dyn × s × cm-5), relative peripheral vascular resistance (RPVR, c.u.). The Kérdö index (KI) was also calculated as follows: KI = 100 × (1-DBP/HR).
The classification of I.K. Shkhvatsabaya et al. distinguishes hypokinetic, eukinetic, and hyperkinetic types of central hemodynamics based on the CI regardless of the sex and age of the subject [3, 8]. The classification of César A. Romero et al. is also based on the CI and systemic vascular resistance (SVR) [9]. However, several investigators argue that CI is not an appropriate indicator for these purposes [2, 10]. Yu.E. Teregulov proposed a method to determine the type of hemodynamics using the percentage of actual CO from the predicted CO (PCO): % CO = 100 × (CO-PCO)/PCO. The PCO is calculated using the N.N. Savitsky formula: PCO (L/min) = basal metabolic rate (BMR)/281, where BMR is the basal metabolic rate influenced by the sex, age, and height of the patient taking into account the intensity of metabolism. BMR is calculated using the Harris-Benedict equation:
where BW is body weight in kg, H is height in cm, and A is the age in years.
In this study, the following definitions of types of central hemodynamics were used [2]:
The mean body weight of the subjects was 61.6 ± 0.91 kg (75.2 ± 2.09 males; 57.8 ± 0.72 females). BMI was calculated using the formula: BMI = m/h2, where m is body weight (kg) and h is body height (cm). The adaptation potential (AP) of the CVS was calculated using the formula: AP = (0.011 × HR + 0.014 × SBP × 0.008 x DBP + 0.014 × age + 0.009 × body weight – 0.009 × height) – 0.27 [11].
The subjects were divided into groups of hypokinetic, eukinetic, and hyperkinetic types of hemodynamics. The evaluated parameters were analyzed in the overall sample and in female and male subsets. Within- and between-group comparisons of the evaluated parameters were performed depending on BMI (BMI < 25 normal; BMI ≥ 25 overweight). None of the subjects in the hyperkinetic type group had BMI ≥ 25, and, therefore, comparisons were made with subjects with BMI < 25 in the hypokinetic and eukinetic type groups. The obtained data were analyzed using Statistica 10.0. The Shapiro-Wilk test was used to assess the normality of the distribution of sample data. The arithmetic mean (M) and standard deviation (SD) are provided for normally distributed parameters, and the median (Me) and upper and lower quartiles (Q1; Q3) are provided for the other variables. Statistical processing included frequency and correlation analyses and analysis of variance. The Kruskal-Wallis test was used to compare several samples, and the Mann-Whitney test was used to compare two samples. The differences were considered significant at p ≤ 0.05.
Hemodynamic parameters were evaluated in 170 medical students with different types of hemodynamics. Sixty-two (36.5%), 103 (60.6%), and 5 (2.9%) subjects had hypokinetic, eukinetic, and hyperkinetic types of hemodynamics, respectively. The proportions of female subjects with the eukinetic type and male subjects with the hypokinetic type were greater (Table 1). None of the male subjects had the hyperkinetic type.
Table 1. Distribution of the types of hemodynamics in the study sample
Sex |
Type of hemodynamics | ||||
| hypokinetic (group 1) | eukinetic (group 2) | hyperkinetic (group 3) | Total | ||
| number (subjects) | males | 28 | 9 | 0 | 37 |
| % per line | 75.7% | 24.3% | 0 | ||
| % total | 16.5% | 5.3% | 0 | 21.8% | |
| number (subjects) | females | 34 | 94 | 5 | 133 |
| % per line | 25.5% | 70.7% | 3.8% | ||
| % total | 20.0% | 55.3% | 2.9% | 78.2% | |
| number (subjects) | total | 62 | 103 | 5 | 170 |
| % total | 36.5% | 60.6% | 2.9% | ||
In contrast to the greater prevalence of the hyperkinetic type among young people previously reported [2, 12], the proportions of subjects with eukinetic and hypokinetic types were greatest in our study. Similar distributions of the types of hemodynamics were reported [13, 14, 15].
HR, SV, CI, CO, PP, RPP, and KI increased from the hypokinetic type group to the hyperkinetic type group (Table 2).
Table 2. Statistical significance of differences (p) in hemodynamic parameters, AP, and KI across the types of hemodynamics
Parameter |
Types of hemodynamics | р |
||
| Hypokinetic (group 1) | Eukinetic (group 2) | Hyperkinetic (group 3) | ||
| HR | 85.7 (78.1, 94.7) | 83.9 (75.3, 90.9) | 99.6 (93.5, 101.2) | 0.017 |
| SV | 55.2 (54.2, 60.6) | 64.0 (60.3, 70.8) | 74.1 (68.6, 79.4) | 0.000 |
| CI | 1.81 (1.55, 2.24) | 2.00 (1.74, 2.23) | 2.83 (2.24, 3.07) | 0.017 |
| CO | 4.3 (4.1, 5.0) | 5.8 (5.2, 6.2) | 7.8 (7.6, 7.8) | 0.000 |
| MBP | 84.2 (80.0, 93.3) | 76.7 (70.0, 83.3) | 75.0 (70.0, 80.0) | 0.000 |
| PP | 39.0 (30.0, 40.0) | 41.0 (30.0, 50.0) | 50.5 (45.0, 60.0) | 0.003 |
| DBP | 70.0 (60.0, 80.0) | 60.0 (60.0, 70.0) | 55.0 (50.0, 67.5) | 0.000 |
| SBP | 109.0 (100.0, 120.0) | 110.0 (95.0, 110.0) | 100.0 (100.0, 107.5) | 0.008 |
| KI | 21.0 (10.7, 30.5) | 23.0 (10.1, 31.9) | 28.9 (18.2, 34.2) | 0.053 |
| RPP | 93.9 (88.5, 104.3) | 86.5 (77.7, 96.5) | 103.5 (90.3, 113.1) | 0.002 |
| RPVR | 44.5 (36.7, 54.2) | 38.9 (32.5, 46.8) | 24.8 (20.4, 36.6) | 0.003 |
| TPVR | 1,322.5 (1,082.2, 1,602.7) | 1,161.3 (987.3, 1,365.1) | 722.3 (690.1, 1,036.4) | 0.003 |
| АP | 2.18 (1.92, 2.33) | 1.94 (1.78, 2.09) | 2.09 (1.79, 2.16) | 0.000 |
Conversely, TPVR, RPVR, SBP, DBP, and MBP decreased from the hypokinetic type group to the hyperkinetic type group. The lowest SV in combination with high TPVR and RPVR was noted in the hypokinetic type group. The highest SV, CO, CI, PP, and RPP with HR as high as 99.6 (93.5; 101.2) bpm were noted in the hyperkinetic type group reflecting wasteful functioning of the CVS. Thirty-seven percent of borderline 32-year-old hypertensives had increased HR, CI, forearm blood flow, and plasma norepinephrine in a study by Julius S. et al [5]. These subjects had elevated self-determined home BP between 5 and 23 years of age, with the hyperkinetic state associated with sympathetic hyperactivity. It is known that activation of the sympathetic system increases the percentage of low frequencies in the spectral characteristics of heart rate variability and correlates with prehypertension in adolescents [16]. DBP and TPVR decreased while HR, CI, SV, and CO increased from the hypokinetic to hyperkinetic type of hemodynamics in a study of young native residents of the Magadan region, with significant increases in SBP up to high normal and prehypertension levels which was interpreted by the authors as region-specific adaptive changes [13].
In the hypokinetic type group, CO is reduced and, therefore, BP pressure is maintained primarily by the increased vascular tone due to the stimulation of baroreceptors. The hypokinetic type is associated with a wider functional range of the CVS and lower energy consumption. Greater variability of cardiorespiratory responses in healthy young subjects of working age with a hypokinetic type of hemodynamics from the Arkhangelsk region was associated with better adaptation [17]. With equal oxygen consumption, healthy young male and female subjects 18–27 years old with a hypokinetic type have lower CO [18].
Hemodynamic responses in subjects with a hyperkinetic type were associated with positive chrono- and inotropic effects. BP is maintained primarily by the volumetric components of blood circulation, i.e., SV and CO. CO is increased due to increases in SV and HR which requires greater energy expenditure and oxygen consumption and is associated with a reduced chronotropic CV reserve limiting adaptive responses. Higher SBP and MBP were reported in young male subjects with a hyperkinetic type [13]. However, in this study, MBP was significantly higher in the hypokinetic type group. MBP is considered to be the perfusion pressure. Yu.E. Teregulov also demonstrated higher MBP and TPVR with lower CI in healthy young subjects with a hypokinetic type [19]. Girls are known to have lower SBP and MBP compared with boys [20], and, therefore, a trend toward lower SBP observed in the hyperkinetic type group might have been due to a greater proportion of female subjects in this group. PP reflects the interaction between the arteria and SV [21] and was shown to be higher in overweight children and young adults with evidence of vascular wall remodeling [12, 22]. In our study PP increases in subjects with a hyperkinetic type compared with those with a hypokinetic type, similar was reported [23]. Higher RPP in students with a hyperkinetic type indicates increased work and reduced maximum aerobic performance of the myocardium with increased energy expenditure and possible evidence of CVS dysregulation. The KI values reported in all study groups suggest the overactivation of the sympathetic division of the autonomic nervous system in students preparing for exams. The controlled system (organism) may become destabilized with the involvement of the central mechanism of regulation [16].
Male subjects in the hypokinetic and eukinetic type groups had differences in PP, SV, CO, and KI. Female subjects in all three groups had differences in HR, PP, MBP, SV, CO, CI, TPVR, and RPVR (Table 3).
Table 3. Statistical significance of the differences in the hemodynamic variables and AP across the types of hemodynamics by sex
Parameters |
Females | Males | ||
| H test | р | U test | р | |
| HR | 9.22 | 0.0099 | 111.0 | 0.6077 |
| SBP | 0.17 | 0.9149 | 126.0 | 0.9858 |
| DBP | 3.3 | 0.1887 | 105.0 | 0.4680 |
| PP | 16.8 | 0.0002 | 60.0 | 0.0204 |
| MBP | 11.3 | 0.0035 | 102.5 | 0.4155 |
| SV | 31.5 | 0.0000 | 51.5 | 0.0088 |
| CO | 72.9 | 0.0000 | 33.0 | 0.0010 |
| CI | 8.1 | 0.0173 | 106.0 | 0.4900 |
| TPVR | 8.1 | 0.0174 | 103.0 | 0.4257 |
| RPVR | 6.7 | 0.0351 | 104.0 | 0.4466 |
| RPP | 4.4 | 0.1108 | 101.0 | 0.3857 |
| KI | 1.3 | 0.5329 | 57.0 | 0.0193 |
| АP | 0.99 | 0.6090 | 106.0 | 0.4900 |
The highest HR (99.6 (93.5; 101.2)), PP (50.5 (45.0; 60.0)), SV (74.12 (68.6; 79.43)), CO (7.76 (7.64; 7.78)), and CI (2.83 (2.24; 3.07)) were observed in female subjects with a hyperkinetic type while greater MBP (83.3 (73.3; 90.0)), TPVR (1311.57 (1060.99; 1446.37)), and RPVR (42.55 (36.6; 49.8)) were reported in female subjects with a hypokinetic type of hemodynamics (Figure 1).
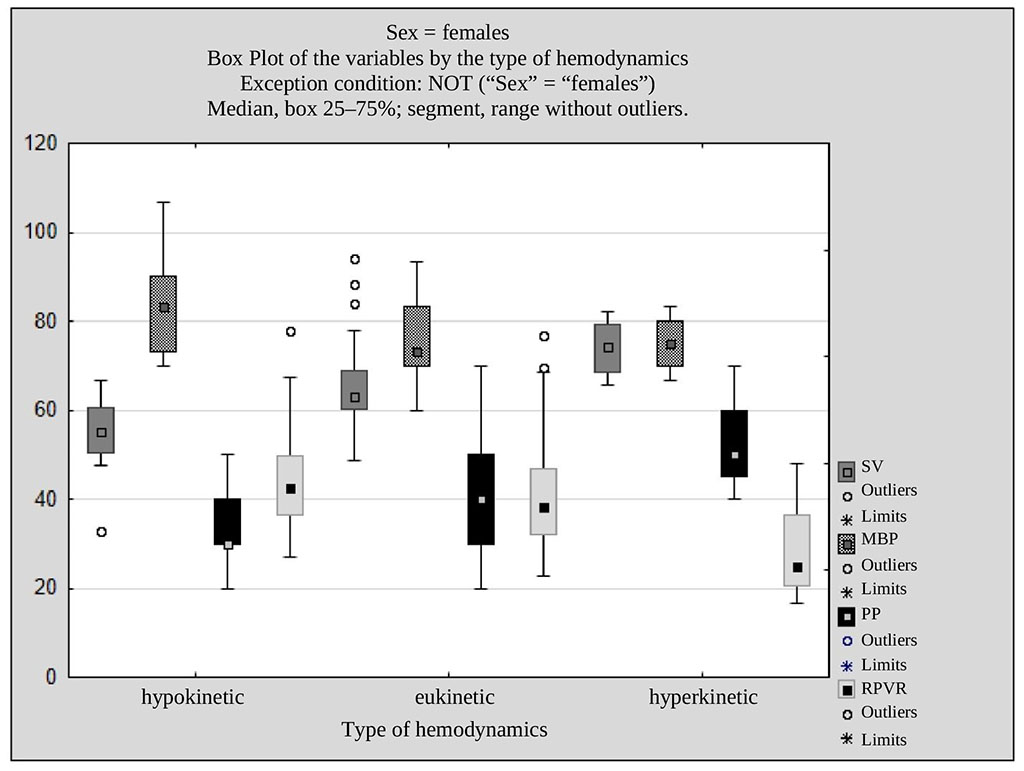
Fig. 1. SV, MBP, PP, RPVR in females across the types of hemodynamics
Male subjects with a eukinetic type had higher PP (50.2 (40.0; 51.0)), SV (65.5 (60.1; 71.3)), CO (6.05 (5.81; 6.41)) compared with males with a hypokinetic type most of whom had increased sympathetic activity as evidenced by KI (24.05 (9.49; 30.49)) (Fig. 2).
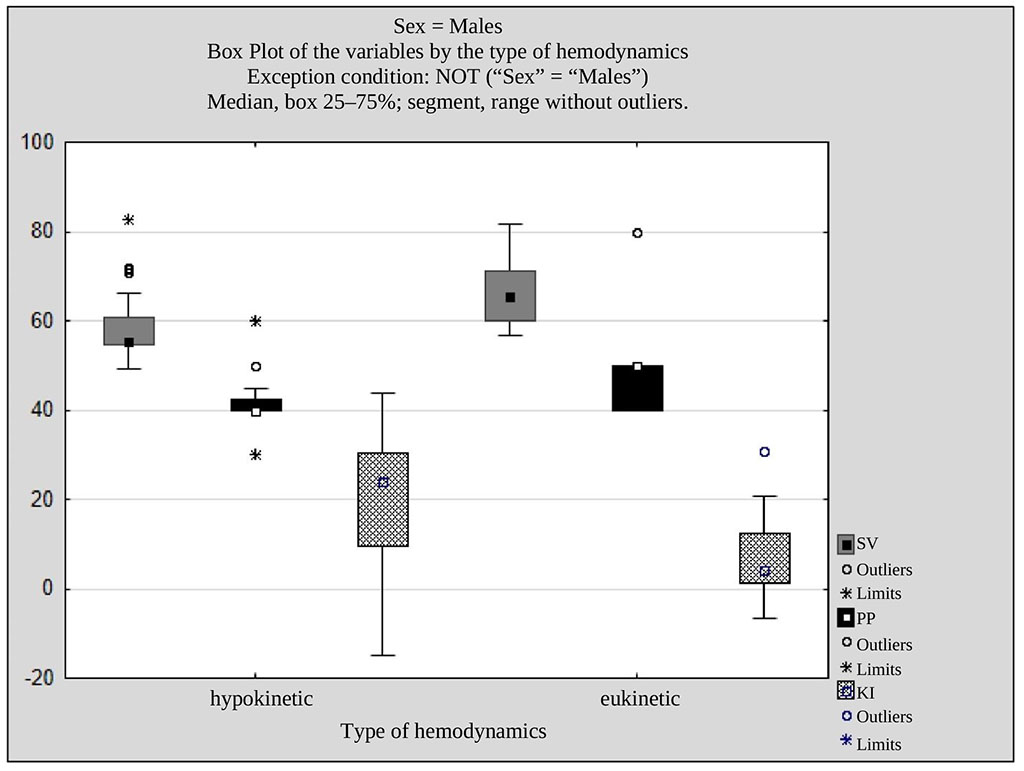
Fig. 2. SV, PP, and KI in males across the types of hemodynamics
The observed within-group trends in most of the evaluated parameters were consistent with types of hemodynamics both in female and male subjects.
Positive correlations were observed between BMI and HR, PP, MBP, RPP, SBP, DBP, and AP (Fig. 3). The figure shows that higher BMI was associated with a significantly greater load on the CVS and higher AP.
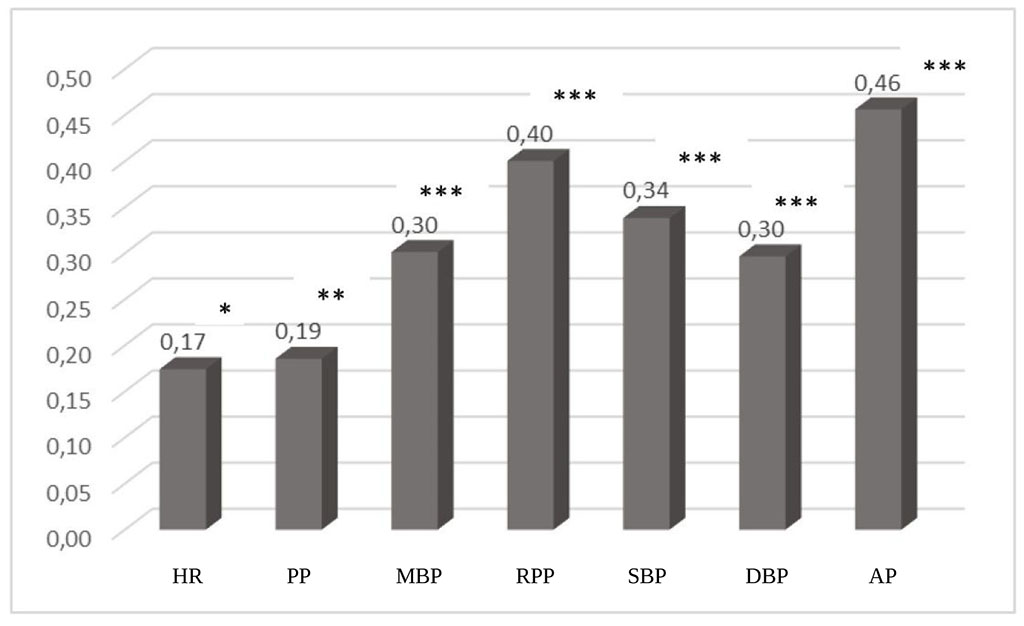
Fig. 3. Spearman correlation coefficients between BMI and hemodynamic parameters (* p = 0.0253; ** p = 0.0215; *** p = 0.0000)
The main hemodynamic parameters across the types of hemodynamics broken down by BMI are shown in Table 4.
Table 4. Hemodynamic parameters and AP across the types of hemodynamics broken down by BMI
| Parameters | Hypokinetic, BMI < 25 | Hypokinetic, BMI ≥ 25.0 | Eukinetic, BMI < 25 | Eukinetic, BMI ≥ 25.0 | Hyperkinetic, BMI < 25 |
| HR | 84.2 (74.1, 92.4) | 91.7 (83.2, 102.7) | 83.3 (75.3, 89.9) | 89.3 (83.6, 93.9) | 99.6 (93.5, 101.2) |
| SBP | 110.0 (100.0, 120.0) | 120.0 (110.0, 120.0) | 100.0 (90.0; 110,0) | 110.0 (110.0, 120.0) | 100.0 (100.0, 107.5) |
| DBP | 70.0 (60.0, 80.0) | 80.0 (70.0, 80.0) | 60.0 (60.0, 70.0) | 70.0 (60.0, 70.0) | 55.0 (50.0, 67.5) |
| PP | 33.0 (30.0, 40.0) | 40.0 (40.0, 50.0) | 40.0 (30.0, 45.0) | 50.0 (40.0, 50.0) | 50.5 (45.0, 60.0) |
| SV | 55.5 (54.4, 60.4) | 55.1 (54.1, 66.0) | 63.5 (60.3, 66.8) | 66.5 (60.4, 76.7) | 74.1 (68.6, 79.4) |
| CO | 4.3 (4.0, 4.6) | 4.7 (4.2; 5.5) | 5.6 (5.1; 6.1) | 6.2 (5.9; 6.8) | 7.8 (7.6, 7.8) |
| CI | 1.8 (1.6; 2.3) | 1.8 (1.6, 2.2) | 2.0 (1.7, 2.2) | 2.1 (1.8, 2.2) | 2.8 (2.2, 3.1) |
| MBP | 83.3 (78.3, 90.0) | 90.0 (80.0, 93.3) | 76.7 (70.0, 83.3) | 76.7 (70.0, 83.3) | 75.0 (70.0, 80.0) |
| TPVR | 1,316.9 (1,048.1, 1,594.3) | 1,337.9 (1,193.8, 1,643.8) | 1,161.3 (1,003.7, 1,366.7) | 1,262.4 (971.0; 1,331.7) | 722.3 (690.1, 1,036.4) |
| RPVR | 43.1 (34.9, 51.9) | 48.1 (38.4, 62.1) | 38.9 (32.7, 46.7) | 39.6 (33.7, 46.8) | 24.8 (20.4, 36.6) |
| RPP | 91.8 (84.9, 99.8) | 102.9 (97.2, 115.9) | 83.7 (76.9, 93.2) | 96.8 (90.9, 106.5) | 103.5 (90.3, 113.1) |
| АP | 2.0 (1.9, 2.3) | 2.4 (2.2, 2.5) | 1.9 (1.8, 2.1) | 2.2 (2.0, 2.2) | 2.1 (1.8, 2.2) |
None of the subjects in the hyperkinetic type group had BMI ≥ 25, and, therefore, comparisons were made with subjects with BMI < 25 in the hypokinetic and eukinetic type groups. Differences in the hemodynamic parameters and AP that were dependent on both the type of hemodynamics and BMI were found (Table 5).
Table 5. Statistical significance of the differences in the hemodynamic parameters and AP by the type of hemodynamics and BMI
| Parameter | HKT: normal BMI vs. HKT: overweight | HKT: normal BMI vs. EKT: normal BMI | HKT: overweight vs. EKT: overweight | EKT: normal BMI vs. EKT: overweight | HKT: normal BMI vs. HrKT: normal BMI | EKT: normal BMI vs. HrKT: normal BMI | HKT: overweight vs. HrKT: normal BMI | EKT: overweight vs. HrKT: normal BMI |
| HR | 0.026 | 0.803 | 0.441 | 0.113 | 0.008 | 0.002 | 0.226 | 0.059 |
| SBP | 0.048 | 0.029 | 0.909 | 0.002 | 0.521 | 0.892 | 0.106 | 0.134 |
| DBP | 0.002 | 0.014 | 0.016 | 0.147 | 0.049 | 0.257 | 0.001 | 0.078 |
| PP | 0.005 | 0.002 | 0.087 | 0.003 | 0.002 | 0.006 | 0.036 | 0.346 |
| SV | 0.069 | 0.000 | 0.004 | 0.284 | 0.000 | 0.011 | 0.001 | 0.203 |
| CO | 0.039 | 0.000 | 0.000 | 0.001 | 0.000 | 0.000 | 0.000 | 0.001 |
| CI | 0.997 | 0.327 | 0.181 | 0.293 | 0.001 | 0.001 | 0.001 | 0.020 |
| MBP | 0.061 | 0.000 | 0.022 | 0.319 | 0.046 | 0.726 | 0.018 | 0.407 |
| TPVR | 0.159 | 0.115 | 0.145 | 0.940 | 0.012 | 0.045 | 0.002 | 0.059 |
| RPVR | 0.168 | 0.067 | 0.097 | 0.975 | 0.011 | 0.054 | 0.002 | 0.078 |
| RPP | 0.001 | 0.100 | 0.365 | 0.001 | 0.129 | 0.032 | 0.733 | 0.800 |
| АP | 0.000 | 0.013 | 0.149 | 0.000 | 0.709 | 0.624 | 0.014 | 0.146 |
Note. HKT, hypokinetic type; EKT, eukinetic type; HrKT, hyperkinetic type; normal BMI, BMI < 25; overweight, BMI ≥ 25.
In the hypokinetic type group, HR, SBP, PP, DBP, CO, RPP, and AP in subjects with BMI ≥ 25 were higher than in those with BMI < 25. In the eukinetic type group, SBP, PP, CO, RPP, АP were also higher in subjects with BMI ≥ 25. Although subjects with BMI ≥ 25 had higher TPVR and RPVR, there were no significant within-group differences.
CI and CO were significantly higher in the hyperkinetic type group than in the other groups regardless of BMI. The maximum CI (2.8 (2.2; 3.1)) and CO (7.8 (7.6; 7.8)) values in the hyperkinetic type group were significantly higher than in the other groups. In the eukinetic type group, overweight subjects had greater SV (66.5 (60.4; 76.7)). Among subjects with BMI < 25, SBP was higher in the hypokinetic type group, and DBP decreased from the hypokinetic to hyperkinetic type; however, overweight subjects with a hypokinetic type had the greatest DBP. With increasing BMI, PP increased in the hypo- and eukinetic type groups peaking at 50.0 (40.0; 50.0) in overweight subjects in the eukinetic type group. This is consistent with the study [22] where excess body weight was associated with higher PP. Higher BMI is also known to have a significant association with higher BP [24. 25. 26]. Overweight subjects with a hypokinetic type had the highest MBP (90.0 (80.0; 93.3)). TPVR and RPVR were the lowest in the hyperkinetic type group than in the hypo- and eukinetic type groups even if compared with overweight subjects from these groups. Overweight subjects in the hypokinetic (102.9 (97.2; 115.9)) and eukinetic (96.8 (90.9; 106.5)) type groups had RPP increased up to the values suggesting reduced reserve and maximum aerobic performance of the myocardium due to increased energy expenditure secondary to increased work of the myocardium. Subjects with a hyperkinetic type had the maximum RPP (103.5 (90.3; 113.1)), even those with a normal BMI.
In the hypo- and eukinetic type groups, AP was higher in overweight subjects (AP > 2.1) suggesting activation of the mechanisms of cardiovascular adaptation whereas subjects with normal BMI had normal AP values (≤ 2.1) that indicates good cardiovascular adaptation.
A eukinetic type of hemodynamics was the most common among medical students during the study period, especially in female subjects, whereas more male subjects had a hypokinetic type.
HR, CO, SV, CI, PP, and RPP increase while TPVR, RPVR, DBP, and MBP decrease from the hypokinetic type to hyperkinetic type of hemodynamics. In the subjects with a hypokinetic type of hemodynamics, TPVR, RPVR, and MBP were involved in maintaining the optimal function of the CVS. Hemodynamic responses in subjects with a hyperkinetic type were associated with positive chrono- and inotropic effects. Subjects with a eukinetic type had intermediate hemodynamic parameters between hypo- and hyperkinetic types. The observed within-group trends in most of the evaluated parameters were consistent with types of hemodynamics both in female and male subjects.
Regardless of the type of hemodynamics, most evaluated hemodynamic parameters and the adaptive potential of the CVS were worse in subjects with BMI ≥ 25 which is an unfavorable predictor suggesting activation of the mechanisms of cardiovascular adaptation.
The author declares the absence of obvious and potential conflicts of interest which must be reported in relation to the publication of this article.